
Poop – it’s not the most glamorous topic, but it’s an important aspect of our health. Believe it or not, the consistency of your poop can provide valuable insights into your digestive health and overall well-being. Let’s talk about why poop consistency matters, what different types of poop can tell us about our health, and how to improve poop consistency for better digestive health.
Poop – it’s not the most glamorous topic, but it’s an important aspect of our health. Believe it or not, the consistency of your poop can provide valuable insights into your digestive health and overall well-being. Let’s talk about why poop consistency matters, what different types of poop can tell us about our health, and how to improve poop consistency for better digestive health.
Understanding Poop Consistency:
Understanding Poop Consistency:
Poop Consistency: The consistency of your poop is influenced by a variety of factors, including diet, water intake, gut health, toileting practices, and lifestyle habits. While everyone’s bowel habits and poop consistency may vary, there are some general guidelines to consider when evaluating the health of your poop.
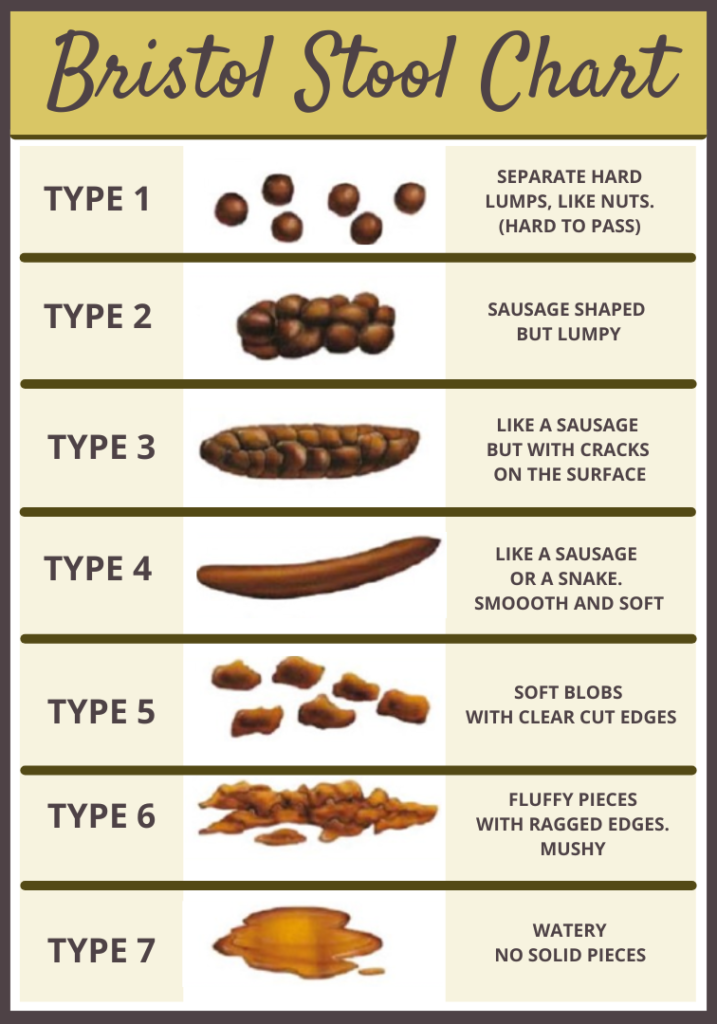
The Bristol Stool Scale: the Bristol stool scale is a medical chart used for assessing poop consistency. Developed by doctors at the University of Bristol, this scale categorizes poop into seven different types based on appearance and texture, ranging from type 1 (hard lumps) to type 7 (entirely liquid). Ideally, poop should fall within types 3 to 5 – soft and easy to pass.
Why Poop Consistency Matters: The consistency of your poop can provide important clues about your digestive health.
Poop Consistency: The consistency of your poop is influenced by a variety of factors, including diet, water intake, gut health, toileting practices, and lifestyle habits. While everyone’s bowel habits and poop consistency may vary, there are some general guidelines to consider when evaluating the health of your poop.
The Bristol Stool Scale: the Bristol stool scale is a medical chart used for assessing poop consistency. Developed by doctors at the University of Bristol, this scale categorizes poop into seven different types based on appearance and texture, ranging from type 1 (hard lumps) to type 7 (entirely liquid). Ideally, poop should fall within types 3 to 5 – soft and easy to pass.
Why Poop Consistency Matters: The consistency of your poop can provide important clues about your digestive health.
Here’s Why It Matters:
Here’s Why It Matters:
Fiber Intake: Fiber is part of food that doesn’t get absorbed into the body.
Insoluble fiber , sometimes called roughage, stays in its same form throughout its journey through your GI tract. It creates texture along the way that scrubs the walls of your intestines, and creates bulk, to give your body something to push along. Insoluble fiber is important for keeping your GI tract clean, and helps your stool form into a long clump. Soluble fiber also does not get absorbed, but passes through the GI tract.
Soluble fiber dissolves in water, and then carries that water with it as it moves through digestion. This brings extra water into the colon where food is formed into stool, the extra water helps keep stools soft and pliable, so it moves through the colon and rectum easily. A diet rich in fiber promotes regular bowel movements and can help achieve optimal poop consistency. Insufficient fiber intake can make it more difficult for your body to push heavy, clay like food through the GI tract and out. Deposits of food stuck to the walls create places for unfriendly bacteria to thrive, and create inflammation and infection known as diverticulitis. Low fiber intake can also cause either, loose stools or constipation. Our body needs a dietary balance for optimal health.
Hydration Levels: Proper hydration is crucial for maintaining overall health, bringing nutrition to cells, and removing waste. When your body is properly hydrated your stools are more likely to be soft and formed. If your stools are not soft and smooth this might be a warning sign of dehydration.
Fiber Intake: Fiber is part of food that doesn’t get absorbed into the body.
Insoluble fiber , sometimes called roughage, stays in its same form throughout its journey through your GI tract. It creates texture along the way that scrubs the walls of your intestines, and creates bulk, to give your body something to push along. Insoluble fiber is important for keeping your GI tract clean, and helps your stool form into a long clump. Soluble fiber also does not get absorbed, but passes through the GI tract.
Soluble fiber dissolves in water, and then carries that water with it as it moves through digestion. This brings extra water into the colon where food is formed into stool, the extra water helps keep stools soft and pliable, so it moves through the colon and rectum easily. A diet rich in fiber promotes regular bowel movements and can help achieve optimal poop consistency. Insufficient fiber intake can make it more difficult for your body to push heavy, clay like food through the GI tract and out. Deposits of food stuck to the walls create places for unfriendly bacteria to thrive, and create inflammation and infection known as diverticulitis. Low fiber intake can also cause either, loose stools or constipation. Our body needs a dietary balance for optimal health.

Gut Health: The balance of bacteria in your gut, known as the gut microbiome, plays a significant role in digestive health and poop consistency. Your gut microbiome is also significantly involved in supporting your immune system. Eating a diet heavy in processed foods, and simple carbohydrates encourages harmful bacteria in your gut to flourish. These bacteria irritate the gut lining, affect absorption of nutrients, and make toxins. Diarrhea, constipation, and mixed stools, can be a sign of imbalances in gut health; a warning sign that your immune system may not be at its best.
Digestive Disorders: Changes in poop consistency can be indicative of underlying digestive disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or celiac disease. Monitoring poop consistency can help identify potential issues and guide further evaluation and treatment.
Pelvic Floor Dysfunction: The pelvic floor muscles control the gate at the bottom of the GI tract. Soft easy to pass stools may not be able to move if the gate is closed from tight or restricted pelvic floor muscles. This causes the stool to stay inside longer, and become harder and drier. If stool is compacted and hard it is more likely to obstruct the bowel. In some cases people strain or push to eliminate hard stool which can cause abrasions, anal fissures, and pelvic organ prolapse. Hard stools, and difficulty pooping can be a sign of pelvic floor dysfunction.
Gut Health: The balance of bacteria in your gut, known as the gut microbiome, plays a significant role in digestive health and poop consistency. Your gut microbiome is also significantly involved in supporting your immune system. Eating a diet heavy in processed foods, and simple carbohydrates encourages harmful bacteria in your gut to flourish. These bacteria irritate the gut lining, affect absorption of nutrients, and make toxins. Diarrhea, constipation, and mixed stools, can be a sign of imbalances in gut health; a warning sign that your immune system may not be at its best.
Digestive Disorders: Changes in poop consistency can be indicative of underlying digestive disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or celiac disease. Monitoring poop consistency can help identify potential issues and guide further evaluation and treatment.
Pelvic Floor Dysfunction: The pelvic floor muscles control the gate at the bottom of the GI tract. Soft easy to pass stools may not be able to move if the gate is closed from tight or restricted pelvic floor muscles. This causes the stool to stay inside longer, and become harder and drier. If stool is compacted and hard it is more likely to obstruct the bowel. In some cases people strain or push to eliminate hard stool which can cause abrasions, anal fissures, and pelvic organ prolapse. Hard stools, and difficulty pooping can be a sign of pelvic floor dysfunction.
Improving Poop Consistency:
Improving Poop Consistency:
Here are several easy steps you can take to improve stool consistency for better digestive health:
- Drink Water: Drink plenty of water throughout the day to maintain hydration levels and promote softer stools. Most find that drinking ½ of your body weight in Ounces is enough to stay hydrated. But it can vary from person to person.
- Increase Fiber Intake: Incorporate fiber-rich foods into your diet, such as fruits, vegetables, whole grains, beans, and legumes. Aim for a mix of soluble and insoluble fiber for optimal digestive health.
- Limit Processed Foods: Minimize consumption of processed foods. They are often low in fiber and can contribute to irregular bowel movements and poor poop consistency.
- Probiotics: Consider taking probiotic supplements or consuming probiotic-rich foods like yogurt, kefir, sauerkraut, Kombucha, and kimchi to support a healthy gut microbiome and improve poop consistency.
- Regular Exercise: Engage in regular physical activity to stimulate bowel movements. Walking, swimming, cycling, and many other activities promote the movement of food through the bowels, and improves overall digestive health.
- Manage Stress: Chronic stress can disrupt digestive function, impact pelvic health and contribute to changes in poop consistency. When your body is in fight or flight mode, it pulls blood away from the gut, and absorption of essential nutrients slows down. If you are in fight or flight mode often, or for extended periods of time, your gut and stool consistency will be affected. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or mindfulness to support gut health.
- Avoid Laxative Abuse: While laxatives can provide short-term relief from constipation, overuse can lead to dependence and worsen poop consistency over time. Keeping your stools very soft and mushy can irritate the mucosal lining of your colon and rectum and perpetuate inflammation, anal fissures, and hemorrhoids. Use laxatives sparingly. If you have been using laxatives for more than 10 days consecutively, it’s time to get help. A Pelvic Floor Physical therapist can work with you to manage your constipation without using laxatives.
Here are several easy steps you can take to improve stool consistency for better digestive health:
- Drink Water: Drink plenty of water throughout the day to maintain hydration levels and promote softer stools. Most find that drinking ½ of your body weight in Ounces is enough to stay hydrated. But it can vary from person to person.
- Increase Fiber Intake: Incorporate fiber-rich foods into your diet, such as fruits, vegetables, whole grains, beans, and legumes. Aim for a mix of soluble and insoluble fiber for optimal digestive health.
- Limit Processed Foods: Minimize consumption of processed foods. They are often low in fiber and can contribute to irregular bowel movements and poor poop consistency.
- Probiotics: Consider taking probiotic supplements or consuming probiotic-rich foods like yogurt, kefir, sauerkraut, Kombucha, and kimchi to support a healthy gut microbiome and improve poop consistency.
- Regular Exercise: Engage in regular physical activity to stimulate bowel movements. Walking, swimming, cycling, and many other activities promote the movement of food through the bowels, and improves overall digestive health.
- Manage Stress: Chronic stress can disrupt digestive function, impact pelvic health and contribute to changes in poop consistency. When your body is in fight or flight mode, it pulls blood away from the gut, and absorption of essential nutrients slows down. If you are in fight or flight mode often, or for extended periods of time, your gut and stool consistency will be affected. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or mindfulness to support gut health.
- Avoid Laxative Abuse: While laxatives can provide short-term relief from constipation, overuse can lead to dependence and worsen poop consistency over time. Keeping your stools very soft and mushy can irritate the mucosal lining of your colon and rectum and perpetuate inflammation, anal fissures, and hemorrhoids. Use laxatives sparingly. If you have been using laxatives for more than 10 days consecutively, it’s time to get help. A Pelvic Floor Physical therapist can work with you to manage your constipation without using laxatives



- Monitor Medications: Some medications, including certain antibiotics, painkillers, and iron supplements, can affect poop consistency. If you notice changes in poop consistency after starting a new medication, Monitor carefully as you implement the suggestions on this list. And contact your prescribing physician.
- Establish a Routine: Aim to have regular bowel movements at the same time each day. Establishing a pattern in the morning when your body is getting started with the day is an excellent way to train your body for optimal poop consistency. While having a bowel movement every day is not a guarantee that your stools will be soft, and easy to pass, having bowel movements LESS THAN every day is a contributing factor to hard dry stools, as more moisture is drawn out of the stool the longer it sits in the colon.
- Be patient on the Pot: Try not to get in a hurry while sitting on the toilet. It is important to soften, and intentionally relax the pelvic floor. This is the gate at the bottom of your GI tract, If your body is trying to push poop through, while your pelvic floor is trying to hold on tight, it affects the feedback loop your body uses to let you know when to go. Take it easy, Relax. Don’t strain and try to force something to happen. Rather allow it to happen, and allow your body to empty completely. If you are clamping off too early, you keep the rest inside, getting harder and drier, and can obstruct movement of normal stool.
- Seek Medical Help: If you struggle with your bowels, if you have persistent problems with constipation or irregular stool consistency this may be a sign that something is out of balance. If you experience changes in poop consistency, accompanied by other symptoms such as abdominal pain, bloating, blood in stool, or unintended weight loss, consult with a healthcare provider for further evaluation and treatment.
- Monitor Medications: Some medications, including certain antibiotics, painkillers, and iron supplements, can affect poop consistency. If you notice changes in poop consistency after starting a new medication, Monitor carefully as you implement the suggestions on this list. And contact your prescribing physician.
- Establish a Routine: Aim to have regular bowel movements at the same time each day. Establishing a pattern in the morning when your body is getting started with the day is an excellent way to train your body for optimal poop consistency. While having a bowel movement every day is not a guarantee that your stools will be soft, and easy to pass, having bowel movements LESS THAN every day is a contributing factor to hard dry stools, as more moisture is drawn out of the stool the longer it sits in the colon.
- Be patient on the Pot: Try not to get in a hurry while sitting on the toilet. It is important to soften, and intentionally relax the pelvic floor. This is the gate at the bottom of your GI tract, If your body is trying to push poop through, while your pelvic floor is trying to hold on tight, it affects the feedback loop your body uses to let you know when to go. Take it easy, Relax. Don’t strain and try to force something to happen. Rather allow it to happen, and allow your body to empty completely. If you are clamping off too early, you keep the rest inside, getting harder and drier, and can obstruct movement of normal stool.
- Seek Medical Help: If you struggle with your bowels, if you have persistent problems with constipation or irregular stool consistency this may be a sign that something is out of balance. If you experience changes in poop consistency, accompanied by other symptoms such as abdominal pain, bloating, blood in stool, or unintended weight loss, consult with a healthcare provider for further evaluation and treatment.
Pelvic floor Physical Therapists are a great resource to identify any physical and mechanical irregularities. Pelvic Floor therapy is a conservative first step to help you sort out your stool consistency and any underlying health concerns.
Pelvic floor Physical Therapists are a great resource to identify any physical and mechanical irregularities. Pelvic Floor therapy is a conservative first step to help you sort out your stool consistency and any underlying health concerns.
Monitor your poop consistency, and monitor your health:
Monitor your poop consistency, and monitor your health:

Poop consistency may not be a glamorous topic of conversation, but it’s an important aspect of our health that shouldn’t be ignored. By understanding why poop consistency matters and implementing strategies to improve it, you can support better digestive health and overall well-being. Remember to listen to your body, stay hydrated, eat a balanced diet rich in fiber, and seek medical attention if you have concerns. If the recommendations on this list do not work for you, consider seeing a pelvic health physical therapist. They help folks get back on track without medications and procedures, and give you tool that last a lifetime. Your gut will thank you!
Poop consistency may not be a glamorous topic of conversation, but it’s an important aspect of our health that shouldn’t be ignored. By understanding why poop consistency matters and implementing strategies to improve it, you can support better digestive health and overall well-being. Remember to listen to your body, stay hydrated, eat a balanced diet rich in fiber, and seek medical attention if you have concerns. If the recommendations on this list do not work for you, consider seeing a pelvic health physical therapist. They help folks get back on track without medications and procedures, and give you tool that last a lifetime. Your gut will thank you!
Are you struggling with bowel movements?
Do you have to strain and push to poop?
Want to know more about what you can do to go #2?
Get the Constipation Relief Guide and start pooping like a pro.
Are you struggling with bowel movements?
Do you have to strain and push to poop?
Want to know more about what you can do to go #2?
Get the Constipation Relief Guide and start pooping like a pro.

Holly McDonald, PT
Pelvic Rehab Specialist
HoHolly McDonald, PT
Pelvic Rehab Specialist
My practice is in Winston Salem NC. I see some patients virtually, but in-person is even better.
I am located at 501 Shepherd St. Winston Salem NC 27103. For more information, or to schedule an appointment please call the office at 336-414-2050, or email us at office@reliefpt.com.
My practice is in Winston Salem NC. I see some patients virtually, but in-person is even better.
I am located at 501 Shepherd St. Winston Salem NC 27103. For more information, or to schedule an appointment please call the office at 336-414-2050, or email us at office@reliefpt.com.






