As soon as I hear someone saying that have been diagnosed with Interstitial Cystitis or Painful Bladder Syndrome, I know what will come next. They tell me, “There is no cure.” It’s as if doctors think of that phrase as part of the diagnosis itself. It’s the phrase that sticks in everyone’s head.
Uncurable, what a hard thing to hear. But the good news is, there is actually a lot you can do to manage those symptoms. And while the doctors might say there is no cure, if you can manage your symptoms to the point where you are pain free, can exercise, have sex, and pee normally- that’s pretty close! Thousands of people have been able to get there. You can too.
What is IC/PBS?
The Definition of Interstitial Cystitis has evolved a bit over the last few decades. Generally, it is pain experienced for at least 3-6 months, anywhere in, around, or near the bladder. The pain gets worse when you have to pee, and gets temporarily better when you release urine. The result is that as soon as your bladder starts to fill, it hurts, and you urgently need to pee. So, you go to the bathroom several times a day. A person without bladder problems will typically use the toilet 4-7 times per day. A person with Interstitial Cystitis or Painful Bladder Syndrome might use the toilet 20 or 40 or even 60 times per day.
Additional symptoms might include burning or pain in the pelvis, bladder, or genitals. Symptoms tend to follow a cycle of flares and remissions.
It affects more women than than men

IC/PBS makes you feel like you have to pee all the time
It is estimated to affect 3.3 million women and perhaps as much as 1.3 million men. Interstitial cystitis is a diagnosis of exclusion, requiring multiple tests to “rule out” other conditions. On average it takes 7 years for sufferers to be diagnosed.
Coping with pain for such a long time can tax other systems on the body. It is not uncommon for people with IC/PBS to also have diagnoses of chronic fatigue syndrome, fibromyalgia, dyspareunia (painful sex), incontinence, IBS, etc.
“Interstitial Cystitis” (IC) was a name given to indicate infection of the tissue around the bladder/urethra. But we have come to understand that it is not an infection, even though many say it feels that way. 10 years ago the term Painful Bladder Syndrome (Or Bladder Pain Syndrome, anywhere but the USA) was introduced as an alternative name. The intent was to gradually shift to PBS, but IC has sort of stuck. For the purposes of this article, I will refer to it as IC/PBS.
What causes IC/PBS?
Many people with IC/PBS can identify a specific event that seemed to be the beginning of their symptoms. Examples might be a UTI, a traumatic event, or an injury. For some, it seemed to start out of the blue.
They don’t know the exact cause of IC/PBS. They do know that, in some cases, people with this collection of symptoms will have small ulcers in their bladder wall called Hunner’s Lesions. There may also be scar tissue in their bladder wall that hurts when stretched.
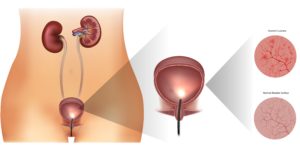
Hunner’s Lesions can be present in the bladder, and may be related to IC/PBS. But the correlation is not clear.
In current medical research, the focus is on improving treatment of these lesions to provide more effective treatments for patients. Surgeries and procedures, such as bladder installations, and techniques to burn the lesions away are among the current practices. There is good evidence that these treatments improve the lesions and offer relief from symptoms.
The problem is, that only about 10% of people suffering from IC/PBS have Hunner’s Lesions. Also, in several studies, it was found that people with no urinary symptoms at all might also have Hunner’s Lesions. So simply addressing the lesions is not a comprehensive approach.
Additionally, 85-90% of patients with IC/PBS also have pelvic floor dysfunction. That is, the muscles and fascia of the floor of the pelvis are not working properly. Usually the muscles are overactive, tight, and super-sensitive. Any touch, stretch, or pull can cause pain and muscle guarding. The bladder and the pelvic floor share nerve innervation. It makes sense that if one area is irritated, then the other can become irritated as well. It can be hard for the brain to pinpoint sensations, and may interpret pelvic floor pain as bladder pain, or vice versa.
What can people do to help their symptoms?
There are a ton of resources online for IC/PBS information. Be careful, it’s quite confusing. You will find out quickly that different sources approach and cover information and treatments very differently.

IC/BPS is usually managed by a specialist
Treatment should include conversations with your doctor. IC might be managed by a Urologist, Gynecologist,
or Urogynecologist, due to the common overlap of symptoms between pelvic pain, genital pain, and bladder pain.
Diet and lifestyle changes
Doctors may recommend modifying diet and lifestyle as a first step to manage IC/PBS. Reducing foods that irritate the bladder (for a list click here) can help calm bladder spasms and nerve sensitivity that is constantly telling your brain you have to pee. Currently there is not one standardized diet established for IC/PBS, but it is widely acknowledged that foods can flare an episode of pain. Elimination diets can be helpful to identify food triggers.
In addition to recommendations from your doctor, find a resource that talks about IC/PBS in a way that resonates with you. When there is information soup, the best advice, is the advice that makes sense to you, so that you can follow it. You will need access to more information that your doctor can provide in his/her short visits. I strongly recommend starting with Nicole Cozean’s book The Interstitial Cystitis Solution. It can be purchased on Amazon. It has good explanations, information and resources that you can apply at your own pace.
Track environmental triggers that flare your symptoms, such as stressors, to help you prepare for, and manage them. Avoid pressure on your waist and abdomen, with looser fitting clothing. Stop smoking.
Your doctor may prescribe medications to help your symptoms, common medications that can help include:
- Nonsteroidal anti-inflammatory drugs,such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), to relieve pain.
- Tricyclic antidepressants, such as amitriptyline (Elavil) or imipramine (Tofranil), to help relax your bladder and block pain by reducing nerve sensitivity.
- Antihistamines, such as loratadine (Claritin, others), which may reduce urinary urgency and frequency and relieve other symptoms.
- Pentosan polysulfate sodium (Elmiron), which is approved by the Food and Drug Administration specifically for treating IC/PBS. They theorize that it helps to protect the inner bladder lining, so that the urine doesn’t irritate it. It can take 2-4 months to begin working, and up to 6 months to see a reduction in urinary frequency.
Pelvic Floor Dysfunction
The hyper-sensitive nerves that innervate the bladder also innervate the pelvic floor muscles. These nerves send pain signals to your brain along the same pathway, using the same nerve roots. It can be difficult for your brain to differentiate between bladder pain, and pelvic floor pain. Overflow from these areas will begin to affect surrounding muscles and fascia in low back, hips, and legs over time. Addressing the pelvic floor dysfunction is crucial to making progress.
Pelvic floor muscles provide support for our bladder, and also help us control the passing of urine, stool, babies, and semen. Pelvic floor physical therapy can provide treatments that address muscle function, reduce spasms and calm nerve activity. With bladder training, and strategies to relax muscles you can reduce pain and muscle tension. Physical therapists specially trained in Pelvic Health can teach you how to perform self-care to improve pelvic floor muscle function and reduce bladder pain, dyspareunia (painful sex), urinary urgency, and frequency.
Pelvic floor physical therapists are also able to spend more time with you and provide direct care. There is more time to answer questions, develop management strategies, and discover related issues that should be addressed. Pelvic PTs can help you with communicating with the rest of your medical care team for better comprehensive care.
Psychological toll of IC/PBS
IC/PBS is a diagnosis of exclusion. Its clinical signature is that there are no clinical findings. Unfortunately, there are some medical practitioners that will then imply that there is no problem. The message to patients is that the pain is imaginary, or a psychological issue. If this has happened to you, I am sorry that you were treated in this way.
Anyone experiencing pain for months or years at a time is bound to have psychological effects. In light of that, counseling can be a helpful component of someone’s recovery team. Counseling can be especially helpful if the onset of symptoms was related to trauma.
Add supplementary treatments
Chronic pain takes a toll on the body, not just in the area that is painful, but all over. Adjunct treatments are really helpful in quieting the angst that is bound to come after coping with pain for extended periods of time. Re-integrating the body and the brain and reducing the state of alarm, as part of a treatment plan, can have profound benefits. Try yoga, acupuncture, massage, shamanic healing, aromatherapy or craniosacral therapy in conjunction with your other strategies to maximize the benefits. It is always an advantage to find practitioners that have experience with people who have IC/PBS.
There is no one recipe for managing IC/PBS. But like baking a cake, there are basic ingredients that will help you get the best results. The ratios of each of the following have to be determined by you.
- Identifying your triggers
- Developing a medical care team
- Lifestyle Changes
- Diet
- Physical Therapy
- Medications
- Adjunct services
- Procedures or Surgeries are a last resort- and only appropriate in some cases.
Don’t give up! It takes a bit of trial and error to find the best recipe to control your symptoms. But it is possible. With the right ingredients, you can take back your life, and enjoy it.
If you need someone to help you navigate the challenges of IC/PBS call and schedule a free consult with Holly McDonald.








